2022.07.03.56
Files > Volume 7 > Vol 7 No 3 2022
Use, knowledge, attitudes and practices of formal and alternative medicine related to Covid-19 in the Ecuadorian population.
1 Genomics Lab. Avd. Amazonas N39-82. Edificio Casa Vivanco, piso 6.
2 Academia Ecuatoriana de Medicina. Quito, Ecuador.
3 Sociedad Ecuatoriana de Genética Humana. Quito, Ecuador.
Available from: http://dx.doi.org/10.21931/RB/2022.07.03.56
ABSTRACT
The Covid-19 pandemic revealed a complex health problem for people and national health systems. Faced with the initial ignorance of the behavior of the SARS-COV-2 virus in populations, people turned to relief and alternative medicines. In Ecuador, the use of traditional or western medicine and the systematic approach of people to conventional medicine are evident realities. Our work aimed to assess the knowledge, attitudes and practices regarding Covid-19 and the use of formal and traditional medicine to treat the disease or contagion. An open, personal and confidential survey was carried out, with 158 questions on general data, ethnicity, health status, covid-19 tests, use of self-medication, use of medicinal plants or other chemical products, and use of antibiotics or antiparasitics, among other data. In the control of the patients, six months after finishing the survey, they were asked about the acceptance of the vaccine and the decision to be vaccinated or not. The results in 3,000 persons (50% female and 50% male) show frequent use of alternative or traditional medicine, even in health personnel or university studies. The study's conclusions reflect that people choose any of the therapies they have access to and even mix traditional treatments with traditional ones that are unproven or toxic.
Keywords: knowledge, attitudes, practices, covid-19, formal medicine, traditional medicine
INTRODUCTION
Ecuador is a very diverse country with a population that is self-defined as mountainous mixed-blood Mestizo (71.9%), African descendants (7.2%), indigenous natives from the Americas (7.1%), coastal mixed-blood Montubio (7.4%), Caucasian (6%) and others (0.4%)1. Regarding the geographic distribution of the population, Mestizos live primarily in urban areas of the country, while indigenous natives from the Americas and African descendants tend to stay in rural areas1. This distribution influences access to health services and reflects deeply ingrained cultural traditions. A previous analysis identified that persons residing in suburban districts and shamans of indigenous communities have little information about conventional Western medicine and knowledge of genetics2. Instead, as in many other countries, they rely on knowledge passed by oral tradition. This traditional knowledge has seen a resurgence and acceptance in the form of alternative medicine in many developing and developed regions of the country3.
In the current SARS-CoV-2 pandemic, research began concerning the virus's epidemiology, genetics and genomics, affected individuals, and especially regarding treatments and vaccines. Institutions have established basic guidelines and policies to protect the community4. Nevertheless, in parallel, a reappearance of popular beliefs is surging to face, prevent and treat COVID5-14.
Medical practices in Ecuador are classified into (a) Formal or Western medicine, (b) Traditional or Native medicine and (c) Popular Non-Formal Medicine. This Non-Formal or non-conventional medicine is known by many other names, including complementary medicine. The WHO recognizes its importance in providing services as a complement or supplement to the already existing health system to deal with disease3.
Within the practices of Popular or Non-Formal Medicine, we find the use of home remedies with the intent to provide an immediate effect and cure, which differs from Western Medicine practice. Both Popular and Traditional-Ancestral medicine credit curative properties to plants and animals. One example of this is the well-known belief of the population of the high mountains of Ecuador that a solid or severe illness needs to be treated with a strong plant to achieve a cure, such as eucalyptus15.
During the pandemic, many challenges were identified, including navigating a complex health system, the event's gravity, intense social and family experiences, prolonged therapeutic interventions, and high cost and death, among others. In this environment, the population searched for curative answers in alternative, non-formal and traditional Native Medicine3, 5-15.
To identify the widespread knowledge developed and seen as helpful against COVID-19, we proposed to evaluate the use of non-formal, alternative and popular practices for individuals affected with the disease. We initiated this evaluation process through information obtained from patient surveys from our Covid Research Project. We ensured meeting all appropriate bioethical standards.
MATERIALS AND METHODS
Three thousand individuals infected with SARS-CoV-2 were surveyed under the Ecuadorian Covid Research Project, which the National Ministry approved of health. Inclusion criteria for individuals to be studied included: having a positive result for infection with SARS-CoV-2 with a qPCR or antibodies (considered time of diagnosis) and a later negative impact once overcoming the acute illness (considered time of cure from the disease). Surveys were obtained for 25 weeks between July and December of 2020, with a one-year follow-up.
Every person surveyed signed informed consent and answered a survey questionnaire of 23 questions that contained general data and demographics, including place of birth, place of residence, gender, age, education level, and clinical data, including symptoms from mild to severe forms of the disease, and specific questions about the management of the illness and overall health status.
Ecuador began the anti-Covid vaccination of the population in 2021, so two additional questions were included in the follow-up, do you agree with the vaccine or not? If you are not vaccinated, would you get vaccinated?
Variables from basic information, clinical data and management of the disease were compared. The analysis was performed in IBM SPSS Statistics v21.0. A value of p<0.05 was considered statistically significant.
RESULTS
Out of the 3,000 participants, 1,500 were male and 1,500 female. The age range was from 14 to 89 years, with a mean of 45 years and a median of 42,5. They were all Ecuadorian natives from 30 different localities and 13 provinces (Figure 1).

Figure 1. Distribution by the province of origin of people infected with SARS-CoV-2.
It was established that the education level was heterogeneous: 3.9% had no educational background, 8.3% had only elementary school instruction, 18.9% had secondary school instruction, 2.2% had technical school training, 47.2% had university training, and 19.5% had postgraduate school training.
Initially, 82% of participants were tested for the detection of the virus at the time of diagnosis, and 74% were later tested at the time of cure with qPCR. Antibodies were initially tested for 18% and 26% of those groups.
Concerning the severity of the illness, 183 individuals (6.1%) were asymptomatic, 1,317 (43.9%) had mild disease, 867 (28.9%) had a moderate condition, and 516 (17.2%) had severe illness. From the latter, 117 (3.9%) individuals died in the hospital.
From the participants, we gathered that 68.3% could identify the person or situation of contagion, 28.9% of cases occurred in employees of health centers and all of those affirmed being infected at work.
Asymptomatic patients learned about their positive results of viral infection after being tested at their place of work. Since they remained asymptomatic, they did not have to receive any treatment and were kept under mandatory quarantine for 14 days, as the national health authority instructed. It is important to note that they were against this compulsory measure as they did not believe they were genuinely infected, had no symptomatology, and remained in good health.
Once they received their positive results, Symptomatic patients maintained isolation due to the virus; 61% of them had between 1 and 14 family members also infected while maintaining this isolation as a family unit (Table 1).
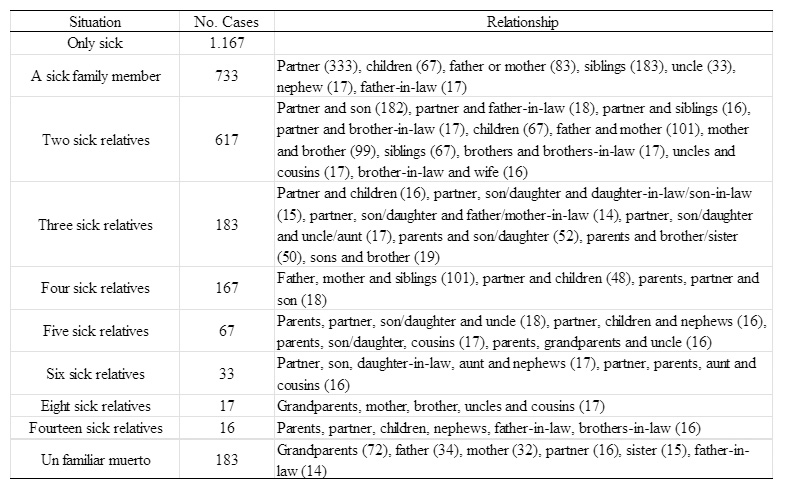
Table 1. The situation of patients and deceased in each patient's home in the study.
All symptomatic patients except two took the recommended treatment for the illness by guidelines: antibiotic, anti-inflammatory medication and anticoagulant. They reported receiving treatment with Azithromycin and acetaminophen for five days. Aspirin was the leading anticoagulant. Most patients did not know that anticoagulant was ordered.
Of the total participants in the study, 69.4% utilized alternative medicine treatments in addition to conventional therapies, especially in the setting of mild to moderate illness. Patients with severe diseases opted to use both therapies only after hospital discharge.
Alternative remedies included vaporizations, herbal waters, juices, deworming, chloride dioxide, alcoholic beverages alone or mixed with diluted herbal-water extracts and visits to a healer (Table 2).

Table 2. Alternative medicine in patients infected with SARS-CoV-2.
Two thousand two hundred patients (73%) expressed the importance of religious practices and divinity as a factor in their healing.
Vaporizations (using steam inhalations) with eucalyptus alone or with as many as eight other herbal combinations were used, including other herbs like chamomile and Rosemary.
The ingestion of medicinal infusions or extracts listed as many as 33 ingredients, with the most common ones being ginger, lemon, honey, cinnamon, chamomile, garlic, onion and lemon verbena. The infusions were prepared with one or many ingredients. The more prevalent combinations included ginger and lemon; garlic and onion; cinnamon and lemon; ginger, lemon and honey; lemon verbena and lemon; and lemon verbena and honey. One hundred seven patients detailed that those infusions used raw cane sugar as a sweetener, not refined sugar, to make it healthier and more palatable.
Some patients put their trust in being cured by drinking natural juices. In contrast, others used alcoholic beverages such as church consecration wine and a variety of moonshine named "Puntas" (which is pure alcohol obtained from sugar cane) in combination with some other plants.
Survey evaluation revealed that other practices were utilized, such as the use of the bovine antiparasitics: Ivermectine in 433 patients (14.4%) and Dectomax (Endectocide) injectable in 33 patients (1.1%). Seventeen patients (0.6%) used oral hydroxychloroquine. Of these, 13.3% of patients had high school education, 50.6% had graduate education, and 36.1% had postgraduate education.
One hundred thirty-three patients were self-treated with Chloride dioxide, including 43 medical doctors and 21 with training as technicians. They mentioned that they had adjusted the dilution concentration depending on the stage of the illness (but no details were provided). Additionally, 117 patients carried around their necks a necklace saturated with chloride dioxide that was procured from Toamit, Japan. This card was the size of an ID card measuring 5.5 x 8 x 0.5cm and was named "Virus Shut Out." The purpose of this card was to create an antiviral halo around the wearer.
Finally, 167 participants visited a naturopathic healer. The treatments by these Shamanic healers often included: "Cleansing from evil influences" by using Guiney pigs, chickens, and rubbing eggs. A "miraculous healing potion" was recommended by all Shamans while also using frequent baths. Vaporizations were used in all patients with moderate to severe symptoms. It was only one healer who recommended the practice of vaporizations.
We looked at the impact of gender with the use of vaporizations (P = 0.346), with other treatments (P = 0.381) and with religious practice (P = 0.50) without finding a statistically significant association. We extended the analysis using educational level in relation to using vaporizations (P = 0.167), other treatments (P = 0.077) and religious practices (P = 0.062) without finding statistically significant differences.
In comparing symptoms and alternative medicine use, we found that vaporizations were associated with dyspnea (P = 0.008) no other statistically significant associations with other symptoms were identified.
To further show that the severity of the disease is essential in the application of alternative therapies, the analysis showed a statistically significant association between the use of vaporizations (P = 0.000) in other treatments (P = 0.001) and religious practices (P = 0.000).
The number of relatives influenced the use of alternative medicine with vaporizations (P = 0.000), with other treatments (P = 0.000) and with religious practices (P = 0.000).
A follow-up took place from July to December of 2021 with all patients. Of those who were symptomatic during the illness, 36.1% had sequelae that included headache so far, back pain, dysgeusia and anosmia (lasting between 1 week and three months) after they had a negative test for the presence of the virus. This symptomatology prompted them to continue using ancestral, traditional and alternative medicines.
Regarding vaccination, 78% of individuals responded that they agreed with immunization, but only 14% stated categorically that they would not be vaccinated.
DISCUSSION
For this research project, obtaining two qPCR or antibodies test results was paramount, one at the beginning with a positive impact on infection and one negative effect to confirm that the virus was no longer present. Participants complained that the test cost was high, with an average of $100 US dollars, while the minimum wage in the country is $398 per month. This occurrence prompted the discussion and request from the government to provide free access to testing as part of its community health plan, as the cost and access to services were prohibitive. Expensive testing did not encourage equal access to testing as in other countries16.
All patients infected with SARS-CoV-2 maintained isolation for the recommended time stated by the treating physician. A minimum of 14 days was prescribed before retesting for the presence of the virus. Nevertheless, 106 patients were required to be isolated for long periods, according to the recommendations of the Ministry of Public Health of Ecuador.
Although our research did not evaluate the clinical therapies provided, it is indispensable to mention what treatments were given. As previously noted, it was common to prescribe Azithromycin and acetaminophen for five days to all patients. 2.2% of patients refused to take those medications because their symptoms were mild and preferred to try alternative therapies. The use of alternative, traditional and ancestral medicine was quite prevalent in patients with COVID infection at 69.4%, which hints at the population's trust in this type of practices. There was no difference in using non-Formal medicine based on gender, age and educational level.
One significant finding previously noted was that 61.1% of participants had between 1 and 14 family members affected by the disease. This occurred despite maintaining appropriate isolation as recommended with distancing, cleaning, and recurrent personal and familial hygiene measures. No information was available to track the infection sequence among those family members. The degree of illness varied among family members; in 182 household families, one person died. These factors: the death of a relative, the lack of formal treatment for the virus, the absence of a vaccine, and limited access to the main health system due to cost appeared to cause individuals to favor alternative therapies (P = 0.000)3, 17.
Regarding vaporizations with Eucalyptus (Eucalyptus globulus & E. citriodora) took place with different degrees of frequency depending on intent for prevention, cure or maintenance of health. Eucalyptus is commonly used to purify the air18 and was introduced in Ecuador in 186019. It is found in a higher percentage in the mountainous provinces of Chimborazo, Pichincha, Loja, Imbabura, Azuay, Cañar and Cotopaxi. Patients use this tree in various ways depending on the leaf type (in recognition of the different species found in Ecuador). Tradition recommends vaporizations with the addition of Chamomile (Matricaria recutita) for the flu and Rosemary (Salvia rosmarinus) for headaches18.
The use of eucalyptus vaporizations by people with dyspnea differs significantly (P = 0.008) from those without that symptom. This effect is consistent with the indication of traditional medicine that recommends it for respiratory conditions18, 20-23.
Ingestion of hot waters (infusions), also known as "homemade waters" or miracle waters, follows a deeply rooted tradition for healing diseases. For the treatment of COVID-19, it contained the main ingredients; lemon, ginger, garlic, cinnamon, onion, lemon verbena, chamomile and honey. COVID is a disease that is felt to be related to being in an unconscious state. Based on traditional beliefs associated with the cosmovision of the illness process, using hot infusions acts as an antagonist or with a counteracting effect17.
Lemon (Citrus limonum) is a medication instead of a food18, 24. It stimulates the immune system, acidifies the body, helps digestion, and cleanses the liver. It is used combined with other ingredients in cold and hot beverages for medical purposes in Ecuador15.
Ginger (Zingiber officinali Roscoe) is seen as a beneficial intervention to alleviate nausea, dizziness, and pain, in addition, to causing an improvement in digestion and fighting the flu, among other indications20, 21. Even though ginger is not a native plant in Ecuador, it has been cultivated in humid tropical and subtropical areas for the last 20 years approximately and quickly became an essential component of healing infusions25.
Of all medicinal vegetables, garlic (Allium sativum) is considered the most extraordinary and compelling for its antibiotic effects, purifying, disinfecting, and anti-cold actions, as well as for relieving congestion and cough18, 20, 21, 24.
An infusion with Cinnamon (Cinnamomum zeylanico) has many medicinal applications and it is recommended to be used in beverages to heal colds18.
On the onion (Allium cepa) there is much popular and even written information about its use and effectiveness against many diseases24. For the flu, the combination with lemon and honey18 is specified, and currently, it has been widely used for covid-19 due to its similarity in symptomatology.
Lemon Verbena (Aloysia citriodora) is called Cedron, Cedar or Verbena by the Indians. This plant is originally from South America, frequently found in gardens and used as an expectorant18. Patients with SARS-CoV-2 mentioned using it often.
Chamomile infusion, one of the most widely used medicinal plants in Ecuadorian coastal and mountainous regions, is used as a febrifuge18.
Honey is seen as an agent that can alleviate fatigue, cough, and sore throat18. Hence, its use was every day among patients with COVID.
Other plants employed less frequently for this illness came from their widespread and ancestral armamentarium. La "borraja" or borage (Borago officinalis) plant is used as an infusion with lemon juice and honey to facilitate expectoration and relieve cold and flu symptoms18. There are testimonies of this plant being used in the mountains of Ecuador for respiratory problems15.
Red Chinchona or Chinchona Bark (Chinchona officinalis and Chinchona pubescens) is the plant from which quinine is obtained to fight malaria. It is recognized as the national plant of Ecuador. It is used for intermittent fevers18 and has been used by Native Americans since before the Spanish Conquistadors came to the Americas. It is a plant at risk of extinction. During the pandemic, patients who were resistant to synthetic pharmacological treatment with Chloroquine and Hydroxychloroquine (anti-malaria treatments) or those unable to access those medications used the plant instead15.
Our research found that most of the many different infusions used also contained two compounds: (1) Impletol, which is the commercial name of the local anesthetic Chlorhydrate of Procaine with caffeine26, and (2) Kaloba, which is an extract of the South African Geranium (Pelargonium sidoides) used to relieve symptoms of the common cold27.
One hundred seven participants used raw cane sugar as a sweetener to make the infusions more palatable. It was very frequently used in Ecuador and obtained by boiling sugar cane18.
Regarding the practice of juicing, some patients utilize fruits such as oranges (Citrus auratium) which is valued as a medicinal tonic to revitalize and cleanse the body18; Tree tomato (Solanum betaceum) with is native of many countries in South America and provide many minerals and vitamins; and tomatoes (Solanum lycopersicum) which is also rich in vitamins like oranges are and is recommended for throat problems18.
Some infusions or waters included Puntas or Moonshine (High-proof distilled alcohol), which was obtained from sugar cane and then distilled following a method passed from generation to generation28.
Despite facing a viral illness, 16.1% of individuals used antiparasitic agents. This was seen as quite surprising, as people who have had high school, university and postgraduate training are aware that this is not an appropriate use of those medications, even more, astounding for that 2.1% of healthcare professionals who did it. It was also surprising that many participants utilized Chloride Dioxide to treat and prevent the disease. This agent is known for its high toxicity29. All the patients who utilized it had previous school and university training. It was even more shocking that 43 physicians also used it. The National Health Authority prohibits the use of Chloride Dioxide due to its toxicity and potential risk to humans.
In searching for a quick cure, many patients visited healers (also known as Traditional Doctors) who prescribed Miracle Waters (see Table 2) and recommended frequent immersion baths to address pain and general malaise. We interviewed a healer who treated many patients who were participants in our study and declared that he had learned this healing wisdom from his father30. The passing of knowledge in this oral and practical way is frequent in the training of urban shamans and the popular culture31.
The survey revealed that 73.3% of participants attributed their healing to religion, metaphysical or magical beliefs. Equally, in the post-illness period, patients with moderate to severe disease continued alternative treatments and respiratory exercises recommended by healers. This Popular and ancestral medicine is quite disseminated in Ecuador17.
The word "Popular Knowledge" referred to knowledge from indigenous native people. "Farmer Knowledge (Campesino)" refers to an ancestral tradition typically obtained by farmers from native people. (i.e., natives from the Andes Mountains)17. A subgroup of participants had popular beliefs that did not come from natives. This subgroup mainly included marginalized socioeconomically poor individuals, whose ideas were usually not considered much by others3. Regardless of origin, 66.7% of Ecuadorian patients with graduate education utilized widespread knowledge in addition to conventional Western medicine. Healthcare workers used Chloride Dioxide and veterinary drugs despite risks and conventional knowledge29.
It is suspected that fear in the face of infected or dying family members played a role in adopting alternative medical treatments, as noted by 2,082 patients.
It is also necessary to note that our population was exposed to a lot of information from the news and social media, which was, in many cases, exaggerated, inaccurate or unverified. This in turn translated into adopting and accepting practices that were not reliable and not effective.
Popular beliefs are natural to humans and allow us to manage our environment with simple interpretations and for specific purposes5, 15, 17. In Ecuador, more than 500 species of vegetables with medicinal use have been identified32, 33. This knowledge of a variety of potential therapies has influenced the attitudes, practices, preferences and trust for specific treatments for the illness caused by this Coronavirus. Approximately 80% of the Ecuadorian population utilizes medicinal plants, folk physical therapies and other natural products daily. Increased availability and low costs are significant drivers in this trend32.
Many myths about vaccines exist and have been widely reported34, 35, and initial fears about the vaccine's benefits have changed over time and the vaccine's safety. Official figures from the Ministry of Public Health of Ecuador36 report that only 14% of individuals do not accept the vaccine or have not been vaccinated. Therefore, the current vaccination statistics are at 78%, and it is expected to reach 90% at the end of the free national vaccination campaign.
CONCLUSIONS
Covid-19 collapsed our world's health system. It showed its weaknesses in dealing with policies and processes regarding public health. In Ecuador, the health system showed severe strain and exhaustion during the pandemic due to its limited infrastructure, slow implementation of security and preventive measures, lack of consistency in maintaining staffing of health workers and inability to see patients. All of these caused people to return to their homes to infect indiscriminately, and in many cases dramatically dying on the streets or right outside hospitals. It is the sum of all those circumstances that contributed to the creation, consolidation and attachment to popular knowledge and practices in facing SARS-CoV-2.
Acknowledgements
The authors thank the following colleagues for referring patients: Dr. Lindsay García and Dr. Mabel Guerra Chum from SOLCA-Matriz Guayaquil, Dr. Ingrid Toapanta from SOLCA-Portoviejo, Dr. Edison Llamuca and Dr. Adrián Fernando Llamuca from Carlos Andrade Marín Hospital-Quito, and Dr. Nadia Karina Marín Naranjo from SOLCA-Quito.
REFERENCES
1. Paz-y-Miño C, Guillen Sacoto MJ, Leone PE. Genetics and genomic medicine in Ecuador. Mol Genet Genomic Med. 2015; 4(1): 9-17.
2. Paz-y-Miño C, Sánchez ME, Sarmiento I, Leone PE. Genetics and congenital malformations: interpretations, attitudes and practices in suburban communities and the shamans of Ecuador. Community Genet. 2006; 9(4): 268-73.
3. WHO. WHO strategy on traditional medicine 2014-2023 (Spanish) [Internet]. Available in: https://apps.who.int/iris/bitstream/handle/10665/95008/9789243506098_spa.pdf;jsessionid=566A0002EE6346E198B3A46518650D15?sequence=1
4. WHO. Coronavirus Disease (COVID-19) Outbreak: Guidance for the Public. (Spanish) [Internet]. Available in: https://www.who.int/es/emergencies/diseases/novel-coronavirus-2019/advice-for-public?gclid=Cj0KCQjw4f35BRDBARIsAPePBHyp96THdqqPRHcKElbD92oQHj8k8PR07aZDNMhEJK6ox5VIQ1P1WPIaAnCFEALw_wcB
5. Pedersen D, Coloma C. Traditional medicine in Ecuador: the structure of the non-formal health systems. Soc Sci Med. 1983; 17(17): 1249-55
6. Lau LL, Hung N, Go DJ, Ferma J, Choi M, Dodd W, Wei X. Knowledge, attitudes and practices of COVID-19 among income-poor households in the Philippines: A cross-sectional study. J Glob Health. 2020; 10(1): 011007.
7. Asmelash D, Fasil A, Tegegne Y, Akalu TY, Ferede HA, Aynalem GL. Knowledge, Attitudes and Practices Toward Prevention and Early Detection of COVID-19 and Associated Factors Among Religious Clerics and Traditional Healers in Gondar Town, Northwest Ethiopia: A Community-Based Study. Risk Manag Healthc Policy. 2020; 13: 2239-50.
8. Rauf A, Abu-Izneid T, Olatunde A, Ahmed Khalil A, Alhumaydhi FA, Tufail T, Shariati MA, Rebezov M, Almarhoon ZM, Mabkhot YN, Alsayari A, Rengasamy KRR. COVID-19 Pandemic: Epidemiology, Etiology, Conventional and Non-Conventional Therapies. Int J Environ Res Public Health. 2020; 17(21): 8155.
9. Yin B, Bi YM, Sun L, Huang JZ, Zhao J, Yao J, Li AX, Wang XZ, Fan GJ. Efficacy of Integrated Traditional Chinese and Western Medicine for Treating COVID-19: A Systematic Review and Meta-Analysis of RCTs. Front Public Health. 2021; 9: 622707.
10. Aprilio K, Wilar G. Emergence of Ethnomedical COVID-19 Treatment: A Literature Review. Infect Drug Resist. 2021; 14: 4277-89.
11. Attah AF, Fagbemi AA, Olubiyi O, Dada-Adegbola H, Oluwadotun A, Elujoba A, Babalola CP. Therapeutic Potentials of Antiviral Plants Used in Traditional African Medicine With COVID-19 in Focus: A Nigerian Perspective. Front Pharmacol. 2021; 12: 596855.
12. Wu XV, Dong Y, Chi Y, Yu M, Wang W. Traditional Chinese Medicine as a complementary therapy in combat with COVID-19-A review of evidence-based research and clinical practice. J Adv Nurs. 2021; 77(4): 1635-44.
13. Rafiqul Islam ATM, Ferdousi J, Shahinozzaman M. Previously published ethno-pharmacological reports reveal the potentiality of plants and plant-derived products used as traditional home remedies by Bangladeshi COVID-19 patients to combat SARS-CoV-2. Saudi J Biol Scie. 2021; 28(11): 6653-73.
14. Trindade AAMD, Lopes Pena PG, Gomes de Lima MA, Freitas MDCS, Araújo KL. Popular health surveillance in traditional fishing communities and the ecology of knowledges in the fight against COVID-19. Cien Saude Colet. 2021; 26(12): 6017-26.
15. Ríos M, Borgtoff Pedersen H. Plants and man. (Spanish) Abya-Yala, Quito, 1991.
16. Quiroz G. How much does it cost to detect the coronavirus in Ecuador and other countries? El Comercio, May 1, 2020. (Spanish) [Internet]. Available in: https://www.elcomercio.com/actualidad/pruebas-pcr-precio-deteccion-paises.html
17. Estrella E. Evolution of medical thought in Ecuador: Medical thought in the pre-Hispanic period. In: Fierro Benítez R. and Ordóñez Nieto G. Ecuadorian Andean and Tropical Biopathology. Volume 1. (Spanish) Academia Ecuatoriana de Medicina, Quito, 1995: 11-29.
18. Arias Alzate E. Medicinal plants. 5th edition. (Spanish) Editorial Bedout, Medellín, 1966.
19. Patzelt E. Flora of Ecuador. (Spanish) Banco Central del Ecuador, Quito, 1985.
20. Silveira D, Prieto-Garcia JM, Boylan F, Estrada O, Fonseca-Bazzo YM, Masrouah Jamal C, Oliveira Magalhães P, Oliveira Pereira E, Tomczk M, Heinrich M. COVID-19: Is There Evidence for the Use of Herbal Medicines as Adjuvant Symptomatic Therapy. Front Pharmacol. 2020; 11: 581840.
21. Grigore A, Cord D, Tanase C, Albulescu R. Herbal medicine, a reliable support in COVID therapy. J Immunoassay Immunochem. 2020; 41(6): 976-99.
22. Gowrishankar S, Muthumanickam S, Kamaladevi A, Karthika C, Jothi R, Boomi P, Maniazhagu D, Pandian SK. Promising phytochemicals of traditional Indian herbal steam inhalation therapy to combat COVID-19 - An in silico study. Food Chem Toxicol. 2021; 148: 111966.
23. Liana D, Phanumartwiwath A. Leveraging knowledge of Asian herbal medicine and its active compounds as COVID-19 treatment and prevention. J Nat Med. 2022; 76(1): 20-37.
24. Capo N. My clinical observations on lemon, garlic and onion. (Spanish) Los libros de la frontera, Madrid, 2013.
25. Oscullo Cattani AP. Feasibility study for the production and commercialization of ginger (Zingiber officinali Roscoe) Hawaiian variety, in San Lorenzo province of Esmeraldas. Thesis of Engineer in Agribusiness. (Spanish) Universidad San Francisco de Quito, 2011.
26. Vademecum. Impletol solution for injection (Ecuador). [Internet]. Available in: https://www.vademecum.es/equivalencia-lista-impletol+solucion+inyectable+1+g%2F50+ml%2B125+mg%2F50+ml-ecuador-n01ba52-ec_1
27. Spanish Agency for Medicines and Medical Devices. Package insert for KALOBA® oral drops. [Internet]. Available in: https://cima.aemps.es/cima/dochtml/p/71733/Prospecto_71733.html
28. Quisaguano D. Typical drinks from Ecuador with alcohol. Paralaseca – The liquor store of the Valley. (Spanish) [Internet]. Available in: https://paralaseca.com/juegos-de-fiesta/blog-bebidas-tipicas-recetas/
29. Couri D, Abdel-Rahman MS, Bull RJ. Toxicological effects of chlorine dioxide, chlorite and chlorate. Environ Health Perspect. 1982; 46: 13-7.
30. Personal communication with Mr. Pablo Betancourt, traditional doctor of the Selva Alegre Naturist Center, Sangolquí, Quito. Available in: https://centro-naturista-selva-alegre.negocio.site/
31. Berenzon S, Saavedra N. Presence of herbalism in the treatment of emotional problems: Interview with urban healers. (Spanish) Salud Ment. 2002; 25(1): 55-66.
32. Buitrón X. Ecuador: Use and trade of medicinal plants. Current situation and important aspects for conservation. (Spanish) [Internet]. Traffic International, Quito, 1999. Available in: https://portals.iucn.org/library/sites/library/files/documents/Traf-061.pdf
33. Cerón Martínez CE. Medicinal plants of the Ecuadorian Andes. In: Moraes M et al. Economic Botany of the Central Andes. (Spanish) Universidad Mayor de San Andrés, La Paz, 2006; 285-93.
34. Travezaño-Cabrera, A. Cabrera-Lliuyac, N. Travezaño-Cabrera, J. SARS-CoV-2 and the myths about vaccination. Enferm Clin (Engl Ed). 2021; 31(3): 199-200.
35. Yeboah P, Daliri DB, Abdin AY, Appiah-Brempong E, Pitsch W, Panyin AB, Adusei EBA, Razouk A, Nasim MJ, Jacob C. Knowledge into the Practice against COVID-19: A Cross-Sectional Study from Ghana. Int J Environ Res Public Health. 2021; 18(24): 12902.
36. Ministerio de Salud Pública. Vacunómetro Covid-19. [Internet]. Available in: https://app.powerbi.com/view?r=eyJrIjoiMjgxODQyZDItMTZiYi00ZjhmLWI0MzEtYWJlNzAxZDcwNWIzIiwidCI6IjcwNjIyMGRiLTliMjktNGU5MS1hODI1LTI1NmIwNmQyNjlmMyJ9&pageName=ReportSection5e050ac003d0b042a320
Received: 17 March 2022 / Accepted: 20 July 2022 / Published:15 August 2022
Citation: Paz-y-Miño C, Leone PE. Use, knowledge, attitudes and practices of formal and alternative medicine related to Covid-19 in the Ecuadorian population. Revis Bionatura 2022;7(3) 56. http://dx.doi.org/10.21931/RB/2022.07.03.56
