2023.08.01.32
Files > Volume 8 > Vol 8 No 1 2023
Assessment of the impact of anemia on hematological parameters among hemodialysis patients with chronic kidney disease
1Environment and Water Directorate, Ministry of Science and Technology, Baghdad, Iraq; [email protected].
*Corresponding author. [email protected], 009647903265918.
Available from: http://dx.doi.org/10.21931/RB/2023.08.01.32
ABSTRACT
Anemia is a common consequence of chronic kidney disease (CKD) that is linked to a decrease in patients' quality of life, a rise in morbidity and mortality, and an acceleration in CKD progression. This study aimed to investigate the hematological profile of chronic renal patients undergoing hemodialysis and to correlate the same with anemia. Fifty (54% males and 46% females) with ages ranging from 18-76 years of patients with CKD and on regular maintenance hemodialysis not less than three months at the Iraqi center for dialysis in Baghdad teaching hospital, and 30 healthy adults were recruited into the study. Hemoglobin concentration, red cell count, white blood cell count, platelet count, ESR, CRP and HCV were assessed for the subjects and controls. Results were analyzed using a t-test independent, and the data were retrieved from the laboratory information system in the hospital. Red blood cell count was reduced in nearly all (96%) of the study patients, while ESR was elevated in (98%) and CRP was elevated in (95%). All patients suffered anemia in HD patients. Most of the patients' WBCs and platelet counts were normal. Anti-HCV antibodies were positive in 15 (30%) of these patients, with non-significant differences in both genders. The study concludes that anemia is a significant comorbidity in hemodialysis patients, with several factors contributing to it, and thorough workup and successful treatment of anemia are essential in this group of patients.
Keywords: Anemia; Hematological profile; Hemodialysis; Hepatitis; chronic kidney disease
INTRODUCTION
Chronic kidney disease (CKD) is a type of kidney disease that causes a progressive loss of kidney function which is present for more ˃ 3 months. 1 Anemia is a common characteristic of CKD associated with poor results in hemodialysis (HD) patients. 2 It is related to a decline in patient quality of life, as well as a rise in morbidity and mortality, and accelerates the progression of CKD. 3 In patients with CKD, anemia is when hemoglobin levels are < 13.0 g/dl in adult males and 12.0 g/dl in adult females. 4 Based on the WHO description, approximately 90% of patients with glomerular filtration (GFR) < 25–30 mL/min would have anemia.5
Kidney disease is the 12th most prevalent cause of death, representing over 1.1 million mortality worldwide per year. 6 According to the Ministry of Health and Environment reports the prevalence of renal failure in Iraq has increased over the last few years. In Iraq, without the Kurdistan region, kidney disease is the fourth among the top ten causes of death at 6.06 %, with 5.9% for males and 5.84% for females. 7 Thus, HD is widely used worldwide, but the effects of HD on patients' blood have not been investigated thoroughly in Iraq.
Patients with CKD undergoing hemodialysis (HD) have higher hepatitis virus compared to individuals with normal renal function. 8 In developing countries, the prevalence of anti-HCV seropositivity among HD maintenance patients varies from 5% to 60% . 9 Therefore, the prevalence of HCV infection in hemodialysis (HD) patients and its associated risk factors is not well established in our country.
This study was carried out on hematological parameters associated with various changes, particularly hemoglobin (Hb) indices, which are most commonly affected, giving rise to anemia. In addition, our country has not well-established the prevalence of HCV infection in hemodialysis (HD) patients and its associated risk factors.
MATERIALS AND METHODS
Patients and Methods
This was a cross-sectional study carried out at the Iraqi center for dialysis in Baghdad teaching hospital, with voluntary participation of 50 (27 males; 23 females) HD patients; it is providing an average of 2 dialysis sessions per week for each patient compared to the control group (30 people non-hepatitis virus without CKD). Inclusion criteria include maintenance HD patients older than 18 years and duration of hemodialysis for more ˃ 3 months.
Ethical Considerations
The local ethics committee of the Ministry of Health and the Environment has approved the research. Written permissions were obtained from the competent authorities based on a description of the study and its objectives, and a signed agreement was reached to treat all individual clinical information as confidential.
Blood Collection
Blood samples were collected from the venous port of the hemodialysis catheter before heparin was added to the blood of regular HD patients. The first 5 IU /ml of blood were discarded to prevent the activation of coagulation due to puncture trauma,10 while the second 5 IU/ml were collected and divided into two parts for the following tests:
1. Hematology tests: blood samples were transferred into tubes with EDTA and used for the following parameters by hematology analyze (China): red blood cell count (RBC) and hemoglobin (Hb) concentration, red blood indices – mean corpuscular hemoglobin (MCH), white blood cell count (WBC), lymphocyte, monocyte, neutrocyte, and platelet count.
2. Erythrocyte sedimentation rate (ESR): according to Biosigma, Italy, blood samples.
3. C-reactive protein (CRP): measured after the serum was separated from blood samples using a (CRP kit, Humen/Germany). es were put into tubes with EDTA and utilized for the ESR test.
4. Rapid Hepatitis C virus test: measured by (SD BIOLINE/ India) after serum separation from blood samples.
Statistical Analysis
Statistical analysis was performed using the Independent sample t-test was utilized to evaluate significant differences. A P-value of 0.05 was considered for the considerable differences between the groups. All statistical analyses were carried out using the Excel 2010 application, and the analyzed data were expressed as a mean ± SD and %.
RESULTS
Hematology Parameters
As indicated in Table-1 for hematology parameters in HD patients, there was no significant difference between males and females in the obtained basic health information, except for the Hb and monocyte at (P˂0.05).
The results show that HD patients comprise 27 males and 23 females, aged 58 ±13.9 for males and 50 ±17.7 for females. Similar results, i.e., a higher number of males with higher age values, were reported in HD patients from several studies in Iraq. 13-'14
Concerning RBCs in HD patients, the majority of patients (96%) (3.06±0.67 10^6μL) were lower than in the healthy control group (4.7±0.68 10^6μL). RBCs of patients showed slight differences in 3.2±0.56 10^6μL for males and 2.98 ±0.77 10^6μL for females in both sexes. In general, most of the findings showed that low RBCs are common in patients with hemodialysis.9
Results appeared all HD patients with Hb levels had anemia (9.05±1.40 g/dL) compared to (13.7±2.7g/dL) in the healthy control group. Hb levels in males (9.2±1.34 g/dL) were slightly higher than in females' dialysis (8.4±1.44 g/dL). At the same time, local standard references are (12 g/dL).
There was a difference compared to the normal value, which might be due to the kidney not making enough of a hormone called erythropoietin that can help the body make red blood cells. 8 In addition, some differences dominated both males and females. Low levels of Hb in females may be due to menstruation every month. For males, the dominant sex hormone is testosterone, and in females, sex hormones are primarily estrogen. Testosterone can increase the rate of metabolism, thereby increasing the rate of Hb formation. 15
Results show that healthy control and hemodialysis patients tend to have average MCH counts of 27.8±4.0 pg and 29.6±2.5 pg, respectively (29.7±2.76 pg males and 29.0±2.2 pg females) relative to the local reference standard (27-33 pg).
In light of the results of this study, it can be concluded that normal MCH in patients during the HD process is due to the administration of several drugs that makes mean capsular hemoglobin normal in HD patients (16). Also, in a previous study done on Chittagong HD patients, Chowdhury et al. showed that MCH was 28.79±3.77 pg. 17
The results of HD patients with WBCs tend to have decreased by 5.3±2.31 10^3μL (4.4±2.25 10^3μL for males and 5±2.35 10^3μL for females) relative to 9.3±2.17 10^3μL for healthy controls. There were 11 (22%) patients with low WBCs, 34 (68%) patients with normal range, and 4 (8%) patients with high WBCs compared to the local standard reference 4-10 10^3μL.
This results in agreement with Kahdina et al., who showed that most patients had normal or even lower WBCs. 15
Furthermore, the majority of patients (68%) with the lymphocyte value (20.6±8.31% for males and 23.7±9.61% for females) were within the normal range, based on local control percentage (20- 40 %). Also, the results show a decrease in monocyte in 44% of HD patients than the local standard reference count (2-8 %). HD patients have a monocyte value of 8.15±3.42 % (8.6±3.66% for males and 7.7 ±3.05% for females), which was higher than 6.03±1.7% in healthy controls. In addition, the results showed that (34 %) of patients had a neutrocyte value (68±21.62 % for males and 68.6±11.17 % for females) above the normal local standard percentage range (40%-60%) in HD people. And there were slight differences in HD patients and the healthy controls group. Overall, HD patients tend to increase the body's defenses, which may be represented by inflammation. 15
In addition, in HD patients, platelet count tends to be reduced in the mean 176.5±66.5 10^3µL, with (166±2710^3µL of males and 187±70.6710^3µL of females) compared with 342±66.9 10^3µL in healthy controls. There were 34% below the local standard reference count (150-4010^3µL). This result is a small percentage relative to another study in which the rate of platelets was estimated at 50 % in HD patients. 18
Furthermore, all HD patients had an ESR of 52±37 mm/hr, which was higher than the usual range according to the local reference standard. The ESR value for HD females was 74±37 mm/hr, which was higher than the 34±27 mm/hr ESR value for males. Statistical analysis showed no significant differences between male and female groups.
In the medical literature, there are just a few reports on the normal range and clinical significance of ESR measurement in HD patients. This is likely because changes in plasma volume caused by dialysis machines have a significant impact on red cell sedimentation. 11 However, ESR levels in hemodialysis blood were enhanced by 98%, whereas Alsomaili et al. found 79.5 % in patients with chronic renal disease .17
Finally, the number of patients with a CRP concentration below a detection level of ≤6 mg/l was 5%. The maximum positive concentration of CRP (≥48 mg/l) was 30±19 mg/l in male and 38±14 mg/l in female patients. Statistical analysis showed no significant differences between male and female groups.
The decreased cost and availability of the CRP test are advantages, especially in underdeveloped nations . 18 Although serum CRP concentrations do not alter with changes in kidney function, serum CRP may be linked to serum albumin levels that are impacted by the inflammatory response in the early stages of renal disease .19
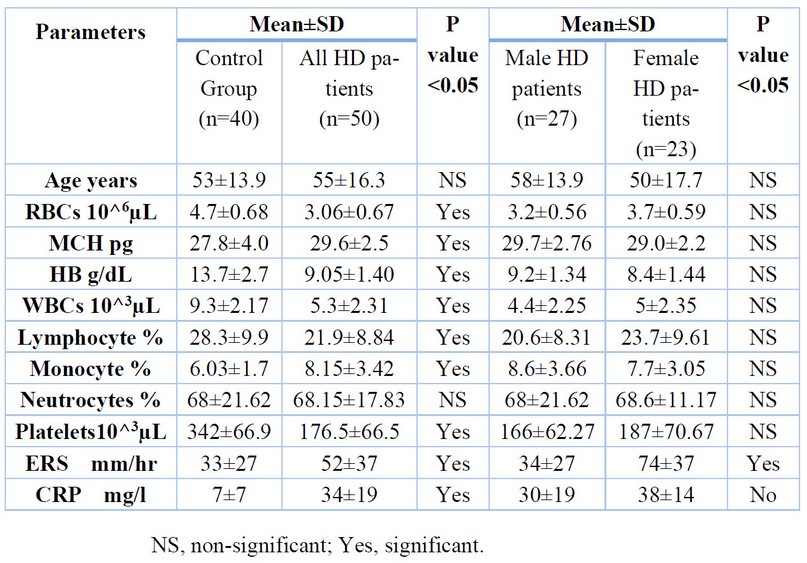
Table 1. Hematology measures of the study patients
Hepatitis C virus in hemodialysis patients
Table-2 shows the results of the hepatitis C virus in HD patients at Baghdad Educational hospital. In general, there were no observed significant differences between both sexes at (P ˂0.05).
In this study, 35 (70%) of the dialysis patients who were not infected with hepatitis C were classified as 20 (74%) for males and 15 (65.2%) for females. The number of patients with hepatitis C virus was 15 (30%); the patients comprised 8 (29.6%) males and 7 (30.4%) females.
In the previous study in the same hospital, the anti-HCV was positive for 12 (7.1%); five (4.9%) were male, and seven (10.4%) were female HD patients. 9 Whereas, similar results, i.e., the prevalence of HCV infection were reported in HD patients in Saudi. 19 In addition, these results agree with Sinjari et al., who showed the exact prevalence of HCV in both male and female hemodialysis patients.20 In general, hemodialysis patients are more vulnerable to such diseases than the general population, which could be returned to blood transfusion is an important factor in the transmission of HCV infection in HD patients, needle sticks, and dialysis workers (if appropriate precautions are not followed). 21

Table 2. Hepatitis C virus measures for hemodialysis patients
Correlation of anemia with some hematological parameters in patients with CKD
Results of the current study show significant differences between anemia and some inflammation, namely RBCs, MCH, WBCs, lymphocyte, neutrocyte, and platelets in patients on regular HD therapy. The correlation coefficient was positive in RBCs, WBCs, lymphocytes, monocyte, ESR while HCV infection showed no correlation coefficient for blood samples collected from HD patients at (P˂0.05), Table 3.
A previous study by Al-Khayat et al. found that anemia for kidney failure was closely associated with hematological parameters (WBC count and granulocyte). 13 While Fouad et al. found in Egypt research in HD patients with hepatitis C viral infection appear to have higher hemoglobin. 23 Therefore, further studies with larger sample sizes are recommended to investigate other hematological parameter and their role in renal anemia.
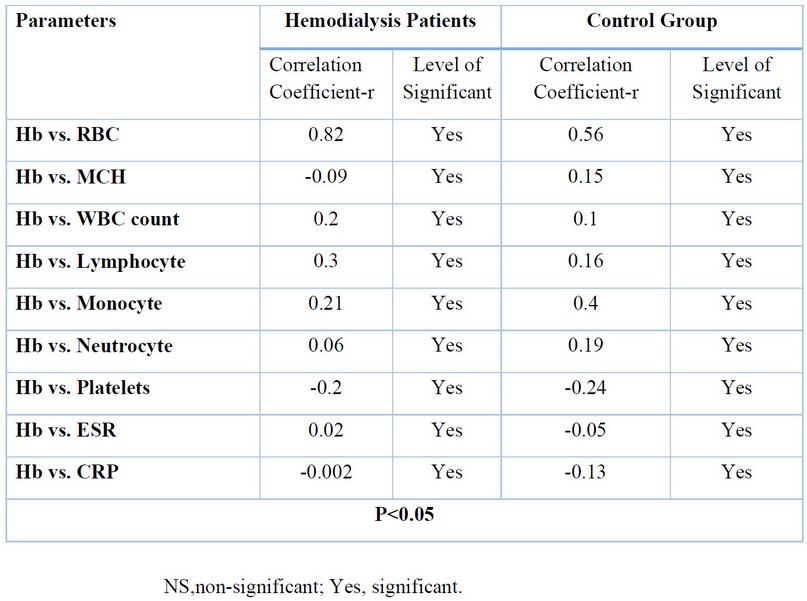
Table 3. Correlation of anemia with some hematological parameters in patients with CKD and healthy group
CONCLUSIONS
Anemia is a leading cause of morbidity in CKD patients and worsens as the disease progresses. The hemoglobin parameter was positively correlated with in RBCs, WBCs, lymphocytes, monocyte, and ESR. Further analysis is required to understand the underlying nature of the observed relationship.
Acknowledgments
The authors would like to thank the staff of central labs and dialysis centers for their continuous support during the study. The authors report no conflicts of interest in this work.
Conflict of Interest
There is no conflicts of interest to declare.
REFERENCES
1. Levin, A and Stevens, P E. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney International. 2013; 85(1) 49-61.
2. Khadayate, R; Piyush, S; Shilpi , S; Siddhi , K. Study of hematological profile in chronic renal failure patients on hemodialysis in a Tertiary care hospital. International Journal of Health Sciences and Research. 2020; 10(12) 1-7.
3. Cases, A; Egocheaga, M I; Tranche, S; Pallarés, V; Ojeda, R; Górriz, J L; Portolés, J M. Anemia of chronic kidney disease: Protocol of study, management and referral to nephrology. Nefrología (English Edition). 2018; 38(1) 8-12.
4. Kopple, J D. National kidney foundation K/DOQI clinical practice guidelines for nutrition in chronic renal failure. American journal of kidney diseases. 2001; 37(1) S66-S70.
5. Sagheb, M M; Fallahzadeh, M A; Moaref, A; Fallahzadeh, M H; Dormanesh, B. Comparison of hemoglobin levels before and after hemodialysis and their effects on erythropoietin dosing and cost. Nephro-urology monthly. 2016; 8(4) e38495.
6. Neuen, B L; Chadban, S J; Demaio, A R; Johnson, D W; Perkovic, V. Chronic kidney disease and the global NCDs agenda. BMJ Globel Health. 2017, Vol. 2, 2, p. e000380.
7. Iraqi Ministry of Health. Annual statistical report 2017. s.l. : Republic of Iraq, Ministry of Health and Environment, 2018; 322.
8. Khattab, O S. Prevalence and risk factors for Hepatitis C virus infection in hemodialysis patients in an Iraqi renal transplant center. Saudi Journal of Kidney Diseases and Transplantation. 2008; 19(1) 110-115.
9. Etik, D O, Ocal, S and Boyacioglu, A S. Hepatitis C infection in hemodialysis patients: A review. World Journal of Hepatology. 2015; 7 (6) 885-895.
10. Frank RD, Müller U, Lanzmich R, Groeger C, Floege J. Anticoagulant-free Genius® haemodialysis using low molecular weight heparin-coated circuits. Nephrology Dialysis Transplantation. 2005; 21(4) 1013-1018.
11. Humudat, Y R, Al-Naseri, S K and Al-Fatlawy, Y F. Assessment of Inflammation, Comorbidity and Demographic Factors in Patients with Kidney Disease in Baghdad. , . Iraqi Journal of Science. 2019;60 (11) 2418-2425.
12. Alyassin, F F. The patient care and complications of hemodialysis procedure for renal failure patients: A descriptive study at Al Nasiriya city, south of Iraq. Journal of Global Pharma Technology. 2018; 10 (03) 356-365.
13. Al-Khayat , H S, Al-Ameri, A M and Abode, M A. Inflammatory status as a contributor for anemia in patients with chronic kidney disease in Karbala, Iraq. Journal of Contemporary Medical Sciences. 2016; 2(8) 123-125.
14. Kahdina, M, Mardiana, N and Fauziah, D. Levels of hemoglobin, leukocytes, and platelets of chronic kidneydisease patients undergoing hemodialysis in Surabaya. Biomolecular and Health Science Journal. 2018;1(1) 29-33.
15. Mikhail, A; Brown, C; Williams, J A; Mathrani, V; Shrivastava , R; Evans, J; Isaac, H; Bhandari, S. Renal association clinical practice guideline on anaemia of chronic Kidney disease. BMC Nephrology. 2017; 18(1) 1-29.
16. Daugirdas, J T and Bernardo, A A. Hemodialysis effect on platelet count and function and hemodialysis-associated thrombocytopenia. International Society of Nephrology. 2012; 182(2) 147-157.
17. Alsomaili, M I; Yousuf, M; Hejaili, F; Almotairi, W and Al-Sayyari, A A. Erythrocyte sedimentation rate in stable patients on chronic hemodiaysis. Saudi Journal of Kidney Diseases and Transplantation.2015; 26(6) 1149-1153
18. Helal, I, Zerelli, L; Krid, M; ElYounsi, F.; Maiz, HB; Zouari, B; Adelmoula, Jand Kheder, A. Comparison of c-reactive protein and high-sensitivity c-reactive protein levels in patients on hemodialysis. Saudi Journal of Kidney Diseases and Transplantation, 2012; 23(3) 477-483.
19. Heidari, B. C-reactive protein and other markers of inflammation in hemodialysis patients. Caspian Journal of Internal Medicine. 2013; 4(1) 611-616.
20. Alsaran,, K A; Sabry, A A; Alghareeb, A H; Al Sadoon, G. Effect of hepatitis C virus on hemoglobin and hematocrit levels in Saudi hemodialysis patients. Renal Failure. 2009; 31(5) 349-354.
21. Sinjari, H A and Bakr, K A. Prevalence and Risk factors of Hepatitis B and C Virus infections among patients undergoing uemodialysis in Kurdistan. Hepatitis Monthly. 2018; 18, 5.
22. Marinaki, S; Boletis, J N; Sakellariou, S; Delladetsima, I K. Hepatitis C in hemodialysis patients. World Journal of Hepatology. 2015;7(3). 548–558.
23. Fouad, M; Ismail, M I; Mahmoud, A A; Fathy, H; Zidan, A; Mostafa, E. Influence of chronic hepatitis B and C infections on anemia in hemodialysis patients. Enliven: Nephrology Renal Study. 2015; 2(1) 001-006.
Received: October 23, 2022 / Accepted: January 15, 2023 / Published:15 February 2023
Citation: Humudat, Y. Assessment of the impact of anemia on hematological parameters among hemodialysis patients with chronic kidney disease. Revis Bionatura 2023;8 (1)32. http://dx.doi.org/10.21931/RB/2023.08.01.32
