2022.07.04.69
Files > Volume 7 > Vol 7 No 4 2022
Sama Al-Shaheeb1 , Husham Kamil Hashim2
, Husham Kamil Hashim2 , Athir Kadhim Mohammed3
, Athir Kadhim Mohammed3 , Haider Abdulkareem Almashhadani4,6*
, Haider Abdulkareem Almashhadani4,6* , Ali Al Fandi5
, Ali Al Fandi5
1 Medical technology institute-Baghdad, Middle technical university, Iraq
2 MOH ministry of health, medical city, national institute of teaching laboratories, Iraq
3 AL-Ma'moon University College, Baghdad, Iraq
4 Department of Medical Laboratory Techniques, Dijlah University College, Baghdad, 10021, Iraq
5Al-Rasheed University College, Dentistry Department, Baghdad, Iraq
6 College of technical engineering, The Islamic University, Najaf, Iraq
*Correspondence author: [email protected] ; Tel.: 009647709988045
Available from: http://dx.doi.org/10.21931/RB/2022.07.04.69
ABSTRACT
Insulin-induced hyperglycemia is the hallmark of diabetes mellitus (DM), including various metabolic disorders. Diabetic people are more likely to develop dyslipidemia, hypertension, and obesity. Type 2 diabetes (T2DM), the most common illness, is generally asymptomatic in its early stages and can go misdiagnosed for years. Diabetes screening may be beneficial in some cases since early identification and treatment can lessen the burden of diabetes and its consequences. This study aimed to find the relationship between Glycated hemoglobin (HbA1c) and lipid profile components in T2DM patients. Methods: This descriptive-analytical and cross-sectional study was performed on the control group and T2DM patients in Medical City in Baghdad between March and June 2021. A total of 90 patients with T2DM and 45 healthy control were included in this study. In the control group, healthy volunteer individuals participated. For all subjects, HbA1c, fasting blood sugar/FBS, and lipid profile (Total Cholesterol/TC, Triglyceride/TG, High-density Lipoprotein/HDL, Low-density Lipoprotein/LDL, and Very Low-density Lipoprotein/VLDL) were assessed. Among T2DM patients, 62.22% (n= 56) were male, and 37.78% (n= 34) were female. Mean ± SD levels of HbA1c, TC, TG, LDL, VLDL, HDL, and FBS were 7.33±0.56 % (168.21±9.23, 146.10±9.64, 137.23±8.32, 41.05±5.86, 43.85±6.17, and 208.81±52.1) mg/dl respectively in the T2DM group. In the control group, the Mean ± SD results of the same parameters were 4.91±0.27%, (171.20±3.57, 116.60±8.25, 105.05±2.11, 41.83±4.92, 44.04±5.54, 96.20±7.8) mg/dl respectively. Results demonstrated statistically significant differences between T2DM patients and control groups in HbA1c (p equal to 0.0025), TG (p equal to 0.015), LDL (p=0.0029), and FBS (p=0.02). Pearson correlation analysis of HbA1c with other variables showed a significant positive correlation with serum TC, TG, LDL, and FBS (r=0.573, P<0.01; r=0.655, P <0.001; r=0.498, P<0.05; r=0.691, P<0.001; respectively). At the same time, the data showed a negative connection between HbA1c and HDL (r= - 0.562, P<0.01). The findings of this study reveal that diabetic people do not have a satisfactory HbA1c level. Furthermore, HbA1c shows a significant correlation with TC, TG, LDL, and VLDL, whereas it has a significant negative correlation with HDL. The study's findings showed that HbA1c might be a useful marker for predicting dyslipidemia in T2DM patients.
Keywords: T2DM, Lipid profile, HbA1c.
INTRODUCTION
Hyperglycemia, which can be induced by insulin production, insulin action, or a combination of both, is the hallmark of diabetes mellitus. Diabetic people have a high chance of developing hyperlipidemia, obesity, and hypertension. T2DM, the most common illness, is generally asymptomatic in its early stages and can go misdiagnosed for years. DM is a long-term metabolic condition brought on by a complicated interplay of genetic, environmental, and behavioral variables. Death rates from diabetes are rising for various reasons, including poor nutrition, obesity, smoking, and physical inactivity 1. Diabetes screening may be beneficial in some cases since early identification and treatment can lessen the burden of diabetes and its consequences2.
Moreover, it was a condition marked by hyperglycemia brought on by a deficiency in insulin action, secretion, or both (insulin resistance) 3. Noncommunicable illnesses affect not just adults but children and adolescents throughout the world4. In both emerging and developed countries, people should be aware of the high rate of diabetes in their populations. In 2012, 1.9 million persons in the United States were diagnosed with diabetes, while worldwide, the prevalence of diabetes was reported to be 8.3%5. An estimated 451 million individuals between 18 and 99 years with diabetes today. According to the latest estimates, nearly half (49.7 %) of patients are undiagnosed. Diabetes implications include coronary heart disease (CHD), peripheral artery disease (PAD), stroke, and other ailments. Endothelial dysfunction will very probably become more common as diabetes rates rise 5.
The long-term glycemic control marker HbA1c is frequently utilized to reflect the typical blood glucose level in diabetics, suggesting the probability of diabetic complications. The HbA1c is currently considered an independent risk factor for cardiovascular disease (CVD) in diabetics and non-diabetics, among other well-established risk factors, including hyperlipidemia and hypertension6. The HbA1c is a valuable diabetes biomarker because it provides information on average blood glucose levels over the last few months7. Monitor glycemic management in people with diabetes by testing their HbA1c. The objective is to go down to less than 7%. Multiple variables can influence HbA1c levels, including sugar intake, exercise, and medication adherence. HbA1c might likely predict dyslipidemia and CVD in some studies 8,9.
The risk of diabetic complications was strongly associated with the leading causes of CVD in diabetics. Cardiovascular disease is one of the primary causes of mortality among diabetes people. As a result, in addition to HbA1c management, it is critical to analyze diabetes patients' blood lipid profiles and take appropriate treatment based on age and type of illness10. T2DM patients are four times as likely than healthy people to die from CVD 11. Diabetic management, early screening, and prompt prevention of diabetes complications dramatically improve disease prognosis and save treatment cost 12. Therefore, our study aimed to estimate the relationship between HbA1c and lipid profile components in T2DM patients.
MATERIALS AND METHODS
This study was performed on control and T2DM patients in Medical City in Baghdad between March and June 2021. In the control group, healthy volunteer individuals participated. Patients with type 1 diabetes, gestational diabetes, or prednisolone-induced diabetes were not acceptable. Ninety patients with T2DM and 45 with control were included in this study. 5 ml of blood was collected from the patients by venepuncture after overnight fasting for 12 hours. Blood samples were divided into two aliquots; the first contains EDTA and is used for the HbA1c estimation. The second one was in a plain tube to collect serum and stored at -20ºC until used. Assessment of FBS and lipid profile were measured by an enzymatic colorimetric method with a commercially available kit (Spinreact, Spain). HbA1c levels measurement was performed with an available kit (Roche, Germany) using Roche Diagnostics Cobas e411 analyzer. These parameters define the DM as having HbA1C ≥ 6.5%, FBS of ≥ 126 mg/dl, and 2-hour plasma glucose levels of ≥ 200 mg/dl (11.1 mmol/l). In a study of the data, the usual descriptive statistics (Mean± Standard Deviation) for the directly measured variables were calculated. The relationships between FBS, HbA1c, and lipid profiles were established using an unpaired t-test. SPSS (Statistical Package for Social Science) version 25.0 was used to analyze the data. p> 0.05 was used as the statistical significance criterion.
RESULTS
The age range for the patients and control groups was between 45 and 70. Among those with T2DM patients, 62.22% (n= 56) were male, 37.78% (n= 34) were female, as shown in (Table 1), and in the control group, 26.67% (n= 12) were male, and 73.33% (n= 33) were female. The mean± SD of age for the T2DM (50.10± 12.86 years) and control group (49.05± 9.66 years) showed no statistical difference (p=0.106).
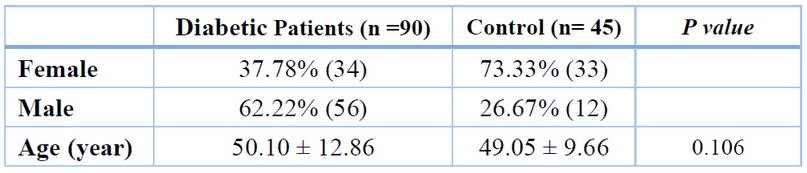
Table 1. Distribution of age and gender in T2DM and control group. Age represents as mean ± SD
Mean ±SD of TC, HbA1c, LDL, TG, VLDL, HDL, and FBS were 7.33±0.56 % (168.21±9.23, 146.10±9.64, 137.23±8.32, 41.05±5.86, 43.85±6.17, and 208.81±52.1) mg/dl respectively in the T2DM group. In the control group, the mean ± SD results of the same parameters were 4.91±0.27%, (171.20±3.57, 116.60±8.25, 105.05±2.11, 41.83±4.92, 44.04±5.54, 96.20±7.8) mg/dl respectively. Results demonstrated statistically significant differences between T2DM patients and control groups in HbA1c (p=0.0025), TG (p=0.015), LDL (p=0.0029), and FBS (p=0.02). On the other hand, the mean ± SD of TC, VLDL, and HDL in serum between study groups showed no significant difference between levels p>0.01, as shown in Table (2) and Figure (1)
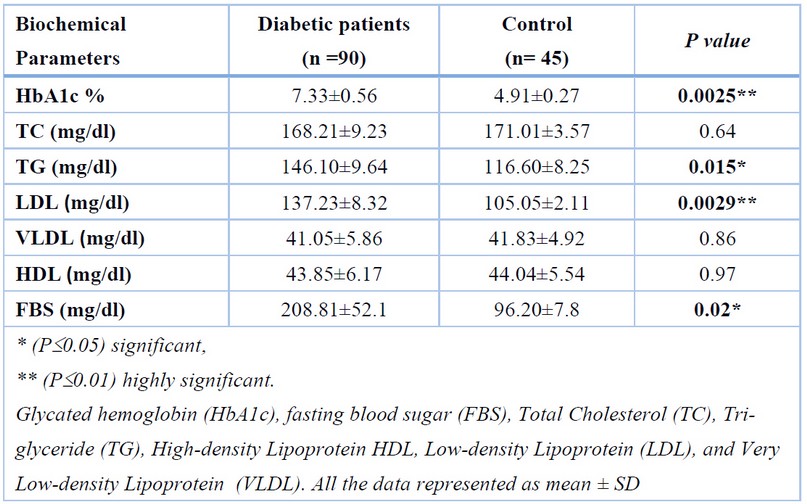
Table 2. Comparison between biochemical parameters (Mean± SD) in T2DM and control groups.
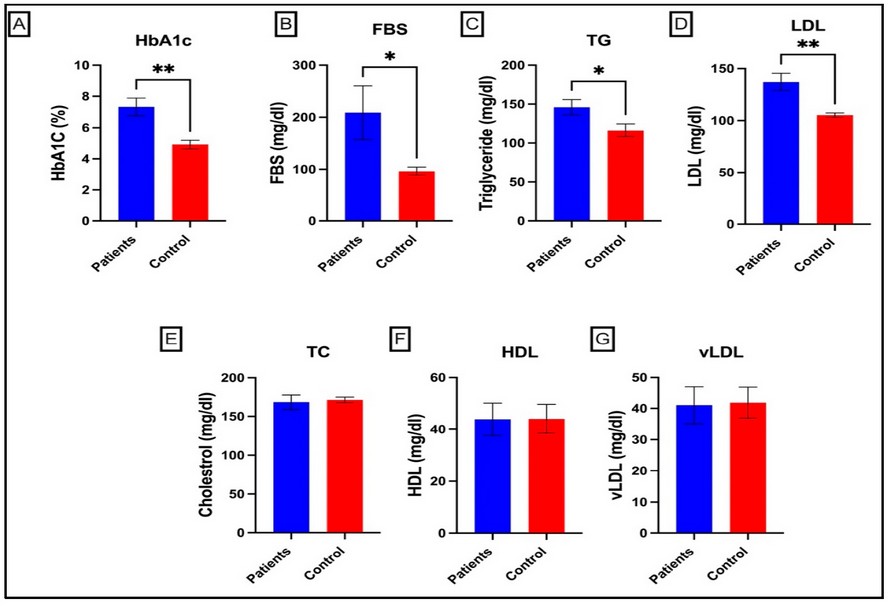
Figure 1. Comparison of biochemical parameters between T2DM and control groups; the highly significant difference between control and T2DM in HbA1c, FBS, TG, and LDL, no significant difference in cholesterol, HDL, and VLDL, independent sample t-test. All data are presented as mean ± SD.
Pearson correlation of HbA1c with other variables revealed a substantial positive connection with serum TC, TG, LDL, and FBS (r=0.573, P<0.01; r=0.655, P<0.001; r=0.498, <P0.05; r=0.691, P<0.001) respectively. While results demonstrated a negative correlation between HbA1c and HDL (r= -0.562, P <0.01), as shown in Table (3)
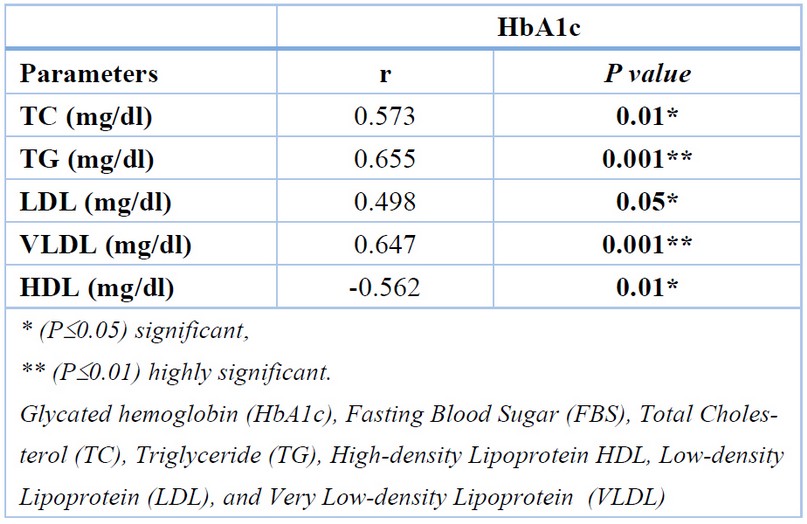
Table 3. Person Correlation analysis between HbA1c and FBS and lipid parameters of diabetic patients.
DISCUSSION
Some lipid profile parameters showed a significant increase in T2DM groups in table (3) many contradicting findings in the literature regarding the correlation between HbA1c and lipid profile parameters. The present study revealed increasing HbA1c levels with an increase in lipid profile parameters like TC, TG, LDL, and VLDL. Moreover, the study demonstrated a negative correlation between HbA1c levels and HDL in DM patients. The positive association between HbA1c and lipid profile parameters has been found in several studies, such as research in Turkey which identified a substantial correlation between TC, LDL, TG, and HbA1c13. According to one study, there is a significant negative connection between HbA1c and LDL 14. Another study stated that HbA1c had no significant correlation with lipid profile except TG 15. HbA1c has been linked to elevated TG levels suggesting that it may predict CVD and is a risk factor in T2DM15.
Based on the results of this investigation, FBS levels were found to be greater than the upper limit for patients with a clinical diagnosis. In T2DM, the HbA1c test is used to check blood glucose management. The HbA1c is a strong predictor of diabetes complications and the length of time a person has had diabetes16. HDL, LDL, TG, and TC levels are well-known risk factors for diabetes complications such as coronary heart disease and CVD. In a study by Rani et al. (2005), when compared to control, FBS and postprandial plasma glucose, TC, VLDL, LDL, TG, and HDL levels were higher in the survey respondents17.
Selvin et al. (2005) studied the relationship between HbA1c and LDL and HDL TC. In addition, our results agree with Selvin et al. (2005) study, which represents that the correlation between HbA1c and HDL was negative, but the correlation between HbA1c and LDL was positive18. Our results go along with a study by Patil et al.,16. People with diabetes often have abnormalities in their lipids, and people with T2DM are no exception. Insulin resistance has previously been linked to the T2DM aberrant lipid profile because insulin resistance causes an increase in fatty acid release, reduces insulin-dependent muscle-free fatty acid uptake, and increases hepatic fatty acid production in the liver19. Diabetic individuals often have high LDL and triacylglycerol values and low HDL. The current investigation results revealed that diabetes individuals had a higher lipid profile. Our study showed a statistically strong positive correlation between HbA1c and lipid profile parameters. Our results are consistent with Wexler et al., 2005 who found that HbA1c and lipid profiles (TC and LDL) have a very positive significant correlation 20; Other researchers have shown a relationship between HbA1c and these lipid profiles in T2DM patients 15, 21.
CONCLUSIONS
According to the results of this study, diabetic people do not have appropriate HbA1c values. Furthermore, HbA1c showed a significant positive correlation with TC, TG, LDL, and VLDL and a significant negative correlation with HDL. In T2DM patients, HbA1c may be a valuable marker for predicting dyslipidemia and CVD.
Financial Disclosure: This research received no external funding.
Competing interests: The authors declare that there is no conflict of interest regarding the publication of this paper.
REFERENCES
1. Mahboobi S, Rahimi F, Jafarnejad S. Effects of prebiotic and synbiotic supplementation on glycemia and lipid profile in type 2 diabetes: a meta-analysis of randomized controlled trials. Advanced pharmaceutical bulletin. 2018;8(4):565.
2. VinodMahato R, Gyawali P, Raut PP, Regmi P, Singh KP, Pandeya DR, et al. association between glycaemic control and serum lipid profile in type 2 diabetic patients: Glycated hemoglobin as a dual biomarker. Biomedical Research (0970-938X). 2011;22(3).
3. Kumar SP, Sandhya A. A study on the glycemic, lipid, and blood pressure control among the type 2 diabetes patients of north Kerala, India. Indian heart journal. 2018;70(4):482-5.
4. Chen L, Magliano DJ, Zimmet PZ. The worldwide epidemiology of type 2 diabetes mellitus—present and future perspectives. Nature Reviews Endocrinology. 2012;8(4):228-36.
5. Group AS. Effects of combination lipid therapy in type 2 diabetes mellitus. New England Journal of Medicine. 2010;362(17):1563-74.
6. Khaw K-T, Wareham N, Bingham S, Luben R, Welch A, Day N. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Annals of internal medicine. 2004;141(6):413-20.
7. Baranwal JK, Maskey R, Majhi S, Lamsal M, Baral N. Association between level of HbA1c and lipid profile in T2DM patients attending diabetic OPD at BPKIHS. Health Renaissance. 2015;13(3):16-23.
8. Naeem M, Khattak RM, ur Rehman M, Khattak MNK. The role of glycated hemoglobin (HbA1c) and serum lipid profile measurements to detect cardiovascular diseases in type 2 diabetic patients. Southeast Asia Journal of Public Health. 2015;5(2):30-4.
9. Kranenburg G, van der Graaf Y, van der Leeuw J, Nature HM, de Borst GJ, Kappelle LJ, et al. The relation between HbA1c and cardiovascular events in patients with type 2 diabetes with and without vascular disease. Diabetes Care. 2015;38(10):1930-6.
10. Ghaemi N, Vakili R. Evaluation of lipids level and its relation to HbA1c in diabetic children. 2005, 15(2):111-117.
11. Saydah SH, Miret M, Sung J, Varas C, Gause D, Brancati FL. Post challenge hyperglycemia and mortality in a national sample of US adults. Diabetes Care. 2001;24(8):1397-402.
12. Arab AG, Zahedi M, Nejad VK, Santiago A, Azimi M. Correlation between hemoglobin a1c and serum lipid profile in type 2 diabetic patients referred to the diabetes clinic in Gorgan, Iran. Original Research Article JCBR. 2018;2(1):26-31.
13. Ozder A. Lipid profile abnormalities seen in T2DM patients in primary healthcare in Turkey: a cross-sectional study. Lipids in health and disease. 2014;13(1):1-6.
14. Samdani TS, Mitra P, Rahim MA. Relationship of glycated hemoglobin with lipid profile among patients with type 2 diabetes mellitus. Bardem Medical Journal. 2017;7(1):43-7.
15. Alzahrani SH, Baig M, Aashi MM, Al-Shaibi FK, Alqarni DA, Bakhamees WH. Association between glycated hemoglobin (HbA1c) and the lipid profile in patients with type 2 diabetes mellitus at a tertiary care hospital: a retrospective study. Diabetes, metabolic syndrome, and obesity: targets and therapy. 2019; 12:1639.
16. Patil M, Kumar N, Nusrath A, Jayaram S, Rajeshwari A. Association of HBA1C with serum lipid profile and lipoprotein (A) in type 2 diabetes mellitus. International Journal of Current Research and Review. 2014;6(6):20.
17. Rani HS, Madhavi G, Rao VR, Sahay B, Jyothy A. Risk factors for coronary heart disease in type II diabetes mellitus. Indian journal of clinical biochemistry. 2005;20(2):75-80.
18. Selvin E, Coresh J, Golden SH, Boland LL, Brancati FL, Steffes MW. Glycemic control, atherosclerosis, and risk factors for cardiovascular disease in individuals with diabetes: the atherosclerosis risk in communities study. Diabetes Care. 2005;28(8):1965-73.
19. Boden G. Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes. 1997;46(1):3-10.
20. Wexler DJ, Grant RW, Meigs JB, Nathan DM, Cagliero E. Sex disparities in the treatment of cardiac risk factors in patients with type 2 diabetes. Diabetes Care. 2005;28(3):514-20.
21. Erciyas F, Taneli F, Arslan B, Uslu Y. Glycemic control, oxidative stress, and lipid profile in children with type 1 diabetes mellitus. Archives of Medical research. 2004;35(2):134-40.
Received: September 22, 2022 / Accepted: October 18, 2022 / Published:15 November 2022
Citation: Al-Shaheeb S, Hashim H K, Mohammed A K, Almashhadani H A, Al Fandi A. Assessment of lipid profile with HbA1c in type 2 diabetic Iraqi patients.Revis Bionatura 2022;7(4) 69. http://dx.doi.org/10.21931/RB/2022.07.04.69
